Pathological Demand Avoidance (PDA)
About Inspire
Inspire Community Outreach Inc. is an incorporated non-profit social services charity providing evidence and culturally informed, family-centered education and programming, designed to meet the needs of those living with mental health issues and neurological/cognitive differences. Charity # 830697231RR0001
Our mission at Inspire Community Outreach Inc. is to support the mental health of children, youth, and families.
Our vision is the development of a community that supports children, youth and families to recognize and celebrate their strengths and potential, and that puts them in touch with resources that benefit their overall well being.
Connecting with us
Please see our website at www.inspirecommunityoutreach.ca to see how we can help, or call 204-996-1547.
Who is this made for?
This is for those caring for and/or living with neurodiversities. We see you and understand the unique challenges, as well as incredible strengths this entails. This will give you an introduction to some information and additional resources surrounding pathological demand avoidance.
Important to know
You may learn some things below that are unfamiliar or feel hard. We understand that it is important to have compassion for ourselves, especially when looking back to times where we didn’t have the information we have today. We are all learning and won’t come to a day where we have all the answers. We all do the best that we can with what we know, and the good news is that we will have opportunities to learn throughout our lives.
Defining Pathological Demand Avoidance
PDA is widely understood to be a profile on the autism spectrum disorder, involving the avoidance of everyday demands and the use of ‘social’ strategies as part of this avoidance. PDA individuals share autistic characteristics and in addition have many of the ‘key features’ of a PDA profile.
Due to its novelty, PDA traits can be incorrectly attributed to a variety of other conditions. Overlaps in characteristics and diagnostic criteria can often make it difficult to ‘target’ exactly what is underlying complex presentations. The most common conditions which may be confused with PDA are: Oppositional Defiant Disorder (ODD), Conduct Disorder (CD), Reactive Attachment Disorder (RAD), Personality Disorders and Developmental Trauma.
It is important to keep in mind that PDA, like many other psychological conditions, is co-occurring. Meaning, there might be more than one thing going on (there almost always is).
PDA is a profile and has various divergent/unique characteristics, such as:
- Being ‘actively passive.’Children with PDA don’t engage with life much and prefer to just watch it pass by. This includes resisting and avoiding the ordinary demands of life. For example, if you hand them something, they might let it drop from their hands with no concern.
- Coming up with excuses.Children with PDA tend to actively avoid demands and often come up with ingenious excuses. This includes using social strategies as part of the avoidance.
- Appearing sociable.Children with PDA may seem quite sociable (at least on the outside), but this may mask differences/difficulties in social interaction and communication.
- Emotionally fragile.Because of their high anxiety levels, children with PDA might quickly switch from passive to aggressive. Children with other types of ASD might have meltdowns, but these aren’t as sudden and happen less often. I.e. having intense emotions and/or mood swings.
- Very imaginative.Children with PDA tend to be comfortable in role play, pretence, or fantasy. This could include for example, role playing by taking on the personality of their favourite cartoon character.
- Social obsessiveness.Children with the PDA subtype usually have social obsessions — i.e., they focus on the demands people place on them and focus on the people around them (real or fictional).
- A need for control. Often driven by anxiety or an automatic ‘threat response’.
- Needing unconventional teaching approaches. Conventional ways of parenting, teaching, or supporting will be ineffective with children with PDA
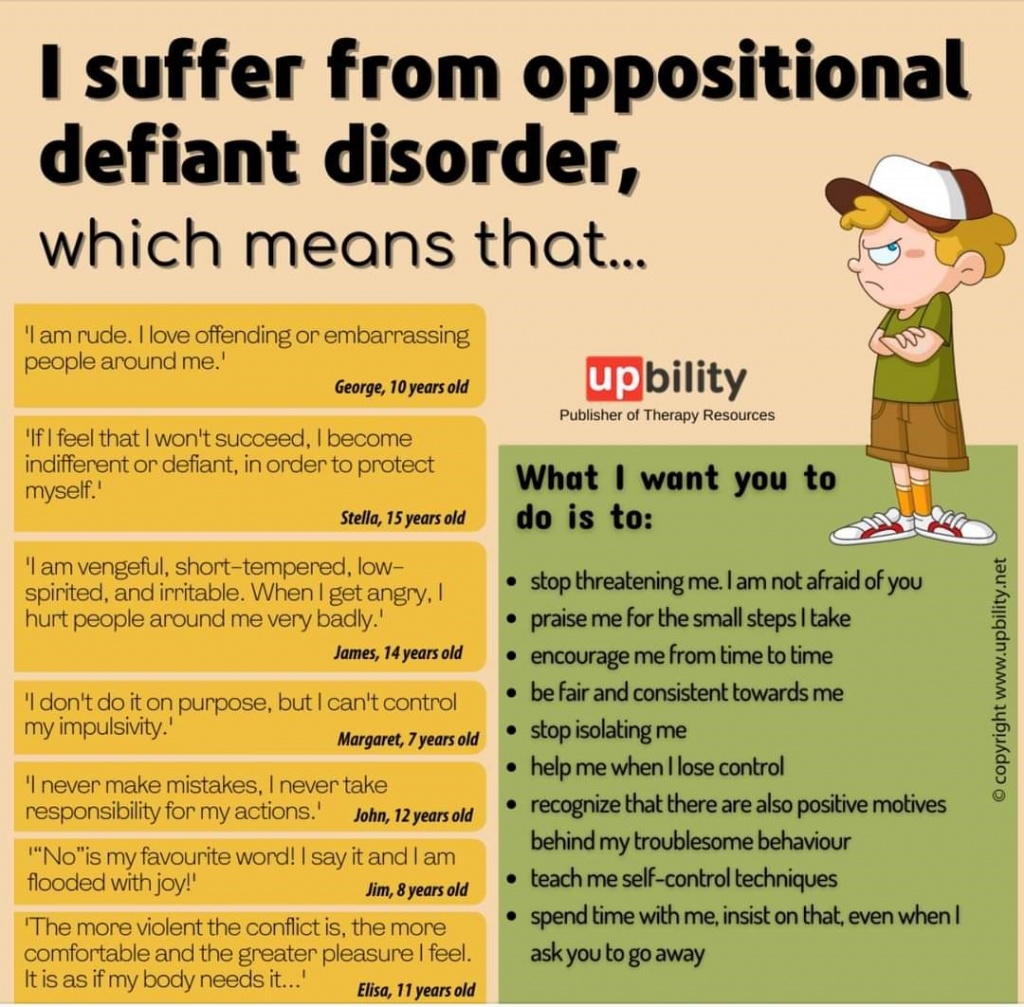
What is ODD Then?
ODD is described as ‘persistent negative, hostile and defiant behaviours’ towards authority. Superficially there may be some similarities with a PDA presentation, however ODD is not an autism spectrum condition. Points of difference include, the fact that the more ‘social’ avoidance approaches seen in PDA (e.g. distraction, making excuses or procrastination) are not usually seen with ODD; and positive parenting courses and reward-based approaches are beneficial for ODD, but ineffective for PDA.
Visual Diagram of What Happens to a Child with PDA When Met With Increasing Demands
Children with PDA feel heightened anxiety when faced with demands. Demands don’t go away and avoidance strategies are rarely 100% effective, so stress and anxiety usually ascends. Due to the main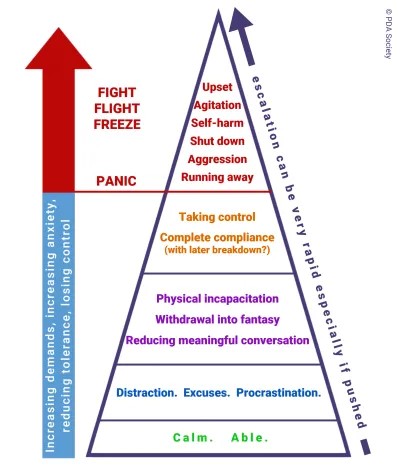 role that anxiety plays in PDA, some individuals with PDA have even called it Pathological demand anxiety. Once the brain of an individual identifies a particular demand as a threat, corticoids increase and the brain looks into its bag of tricks to avoid the demand. It may resort to lying, role playing, ignorance, social manipulation, or just about anything else so that it can protect against whatever the perceived threat is. If those tools don’t work, the brain escalates further up the ladder. And as seen in the hierarchy on the slide, individuals may eventually reach panic mode, which gives three main options for survival: freeze, fight or flight. In a normal setting this often looks like the silent treatment, tantrums, running away, aggression or self-harm. Sadly, this overwhelmed state can be quite common for those with PDA, when they have not been diagnosed and/or are simply misunderstood by the people around them.
role that anxiety plays in PDA, some individuals with PDA have even called it Pathological demand anxiety. Once the brain of an individual identifies a particular demand as a threat, corticoids increase and the brain looks into its bag of tricks to avoid the demand. It may resort to lying, role playing, ignorance, social manipulation, or just about anything else so that it can protect against whatever the perceived threat is. If those tools don’t work, the brain escalates further up the ladder. And as seen in the hierarchy on the slide, individuals may eventually reach panic mode, which gives three main options for survival: freeze, fight or flight. In a normal setting this often looks like the silent treatment, tantrums, running away, aggression or self-harm. Sadly, this overwhelmed state can be quite common for those with PDA, when they have not been diagnosed and/or are simply misunderstood by the people around them.
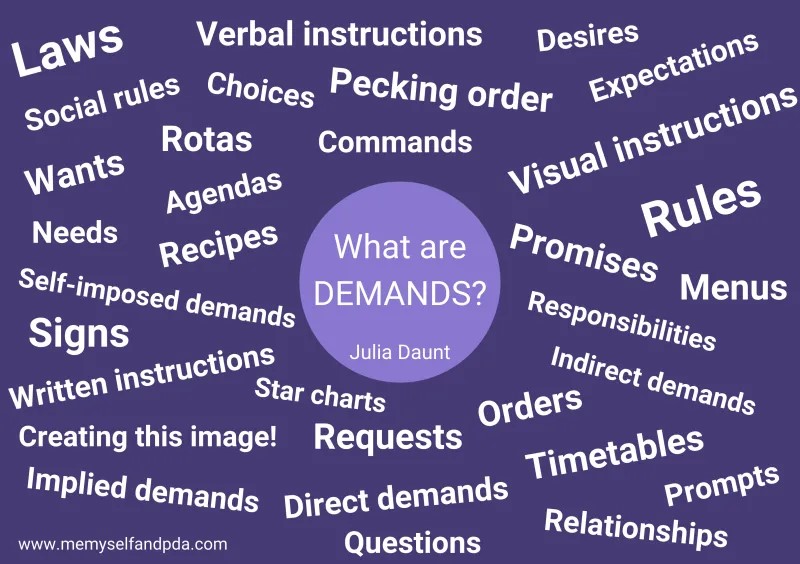
Demands Come in All Shapes and Forms
Some demands seen here don’t even seem like demands, such as: timetables, needs, and pecking order. But they are demands as well! Behind all demands there is some sort of expectation and behavioral implication.
Some common forms of demands with examples are:
- Direct demands/questions (e.g. Turn left here. Hand that to me.)
- Indirect demands/praise/expectations/time (e.g. the chicken will be cooked in 1 hr. You ‘re doing really great finishing your homework!)
- Demands within demands aka. Smaller implied demands (e.g. Going the post office requires getting dressed, getting in your car, driving, interacting with people, etc.)
- Daily life (e.g. taking a shower. Brushing your teeth.)
- Internal demands/thoughts/wishes (e.g. hunger, need for human interaction)
- Things we want to do (e.g. Go outside. Play our favorite instrument. Call your friend.)
 What Parenting Approaches Can Help PDA?
What Parenting Approaches Can Help PDA?
The approaches that help PDA can seem a bit unconventional: a partnership based on trust, flexibility, collaboration, careful use of language and balancing of demands works best. To remember this try the acronym PANDA:
Pick battles
Anxiety management
Negotiation and collaboration
Disguise and manage demands
Adaptation
Strategies to Help Support those with PDA
Firstly, it is important to note that a good relationship goes a long way, therefore one should spend time getting to know the PDA individual better, whether you are their clinician or parent. Secondly, as we have already touched on, everyone is unique! There is no, one size fits all approach, and therefore once a relationship is built, supporting individuals should exercise intuition. Thirdly, one can never go wrong using calm and level emotions.
Now, as far as phrasing demands, one might use complex language to lead into a demand. It’s hard to refuse something when you don’t know what you are really being asked. Novelty and variety can also work well used alongside flexibility and adaptability. Disguising demands has been particularly useful through the use of role playing specifically.
Lastly, potentially less helpful (but good when used in tandem with the previous approaches just mentioned) visual structures can be really helpful, such as including ground rules which are displayed on the wall so that you can refer to them.
Useful Ways of Concealing Demands
- Would you do…
- Could you…
- If you’re happy to…
- When you have finished with…could you…
- Do you mind going/doing…
- Is it ok with you…
- How do you feel about…
- I wish I knew someone who could help with…
- Look at that, now it’s time to…
- You choose, what job shall we do next…
- I bet you can’t do…in five minutes
Reducing anxiety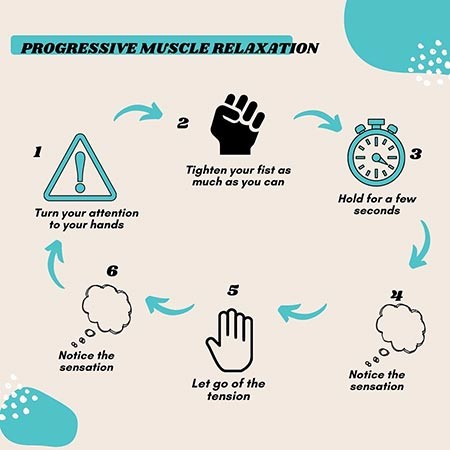
The main issue in young people with PDA is anxiety and if you are able to reduce this, maladaptive behaviours may reduce in severity. Various anxiety reduction techniques can be used when PDA individuals become overwhelmed:
- Stress reduction breathing
- Meditation
- Removal from the situation
- Progressive Muscle Relaxation (PMR)
Other approaches which may be useful are speaking in the third person, requesting rather than demanding and offering a choice of two. Finally, depersonalising a demand may help, such as ‘the whole family are going to’.
Further Reading/Resources
Lived Experience Caregiver Blog About Children Living with PDA
Blog/Website: www.stephstwogirls.co.uk
Autism Parenting Magazine
Online Magazine: www.autismparentingmagazine.com
Me, Myself, and PDA
A Lived Experience Blog Written by an Adult Living with PDA: Blog: https://memyselfandpda.com/
Educational Video on PDA
Youth discussing what is PDA, how it affects them, and the strategies they use to manage it: https://youtu.be/y4H3dvukRC8
Introduction to PDA Video
https://www.youtube.com/watch?v=diHUmhPWXUY
PDA Society Resource
What is PDA, life with PDA, resources, working with PDA, and events & training opportunities: www.pdasociety.org.uk
About Inspire Community Outreach
Inspire Community Outreach (Inspire) is an incorporated non-profit social services charity providing evidence and culturally informed, family-centered education and programming, designed to meet the needs of those living with mental health issues and neurological/cognitive differences.
At Inspire, we support youth and families with unique challenges, while celebrating strength. Programs are designed to meet the needs of those living with mental health issues or neurological/cognitive differences. Inspire’s support is created by the community; from children who grew up with differences, families that include children with differences, and evidence from a clinical perspective.
Compassion. Inclusion. Education.
About the Founder
Angela Taylor is our Founder and CEO. She has a Bachelor of Arts degree from the University of Manitoba, with a major in Psychology and a minor in Sociology and a Post Bacc in Education, focusing on inclusion. She has her Master’s in Disability Studies from the University of Manitoba and is currently completing her PhD in complex families and wraparound care. She is a Mental Health and Accessibility Expert with an eclectic therapeutic approach that includes attachment, cognitive behaviour therapy, positive psychology and CPS model (Collaborative & Proactive Solutions) supports.
We’d love to hear from you!
References
https://www.communitycare.co.uk/2019/05/15/pathological-demand-avoidance-social-workers-need-know
https://www.theedpsych.com/blog/what-is-pathological-demand-avoidance-pda
